Abstract
BACKGROUND: Waldenström macroglobulinemia (WM) is a lymphoplasmacytic lymphoma with a serum monoclonal IgM. Early asymptomatic stages include IgM monoclonal gammopathy of undetermined significance (MGUS) and smoldering WM (SWM). While most IgM MGUS patients (pts) will not progress during follow-up, a greater proportion of SWM pts will do. Most prognostic models identify high-risk SWM; however, they fail to characterize IgM MGUS and low-risk SWM. Moreover, data is scarce regarding how IgM MGUS and SWM survival trends have evolved during the last decades. We wondered whether inclusion of new biomarkers could improve progression risk models using the largest cohort of IgM MGUS and SWM reported. Here, we describe a comprehensive proposal to model progression risk and give more insight into the survival trends of IgM MGUS and SWM using retrospective data from 13 Spanish hospitals.
METHODS: Diagnostic criteria were defined by the Second International Workshop. MYD88 L265P was analyzed by allele-specific or digital droplet polymerase chain reaction. Progression free survival (PFS) was calculated from the date of diagnosis to last follow-up or disease progression (symptomatic WM, other non-Hodgkin lymphoma or AL amyloidosis). Overall survival (OS) was calculated up to death from any cause. To find the best model, we first used a backward stepwise regression with meaningful variables as continuous. Also, a logistic and lasso regression (least shrinkage and selection operator) selected important variables that predicted progression at 10 years. We then categorized continuous data according to Liu and Youden methods. Relative survival (RS) was calculated using the Ederer II method leveraging the Human Mortality Database.
RESULTS: 915 pts (462 IgM MGUS and 453 SWM) were included. Median age at diagnosis was 70 years. 102 (11%) pts were diagnosed before the year 2000. MYD88 L265P (available in 465 pts) was detected in 107 (54%) IgM MGUS and 217 (81%) SWM pts. After a median follow-up of 6 years, disease progression was documented in 250 pts (16% in IgM MGUS and 39% in SWM). The incidence rate of progression per 100 person-years was 2.9 (95% confidence interval [CI] 2.4 - 3.7) and 7.0 (95% CI 6.1 - 8.2) in IgM MGUS and SWM, respectively. Continuous (serum IgM, IgG, IgA, albumin, β2-microglobulin, bone marrow infiltration [BM]) and categorical (MYD88 L265P) candidates to clinical significance were fitted into a backward stepwise regression. Low IgG (hazard ratio [HR] 0.92; p=0.03), high IgM (HR 1.03; p<0.01), high BM infiltration (HR 1.02; p=0.01), and low albumin (HR 0.37; p<0.01) were selected. As the median follow-up of our series was 6 years, we also performed lasso to select predictors of progression at 10 years. Here, all previous variables were selected plus low IgA. We then chose the 4 best predictors between the two methods (BM infiltration, IgM, decreased IgG/IgA, and albumin).
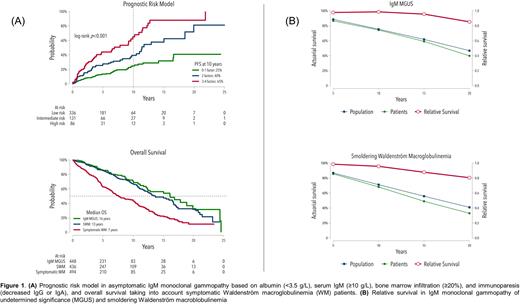
To fit into an easy-to-use model, we categorized continuous data as meaningful for clinicians. Albumin (<3.5 g/L) and IgG/IgA (<6.8/0.6 g/L) were categorized below the normal values; BM infiltration (≥ 20%) and IgM (≥ 10 g/L) cutpoints were established as previously described. 553 pts were introduced in the final model. Each variable was assigned a point so that low (0-1), intermediate (2) and high-risk (3-4) groups were able to discriminate pts. 84% of IgM MGUS pts were categorized as low-risk, while 57% of SWM were intermediate or high-risk. Regarding OS, there were no differences between IgM MGUS and SWM; however, each stage clearly differed from that of series of symptomatic WM pts from the same hospitals (p<0.01) (Figure 1A).
Regarding survival trends, IgM MGUS had a RS slightly higher than that of the matched general population during the first 10 years of diagnosis, with a subsequent decline especially at 20 years. SWM had a RS lower than the general population, with a difference observed from the first 10-15 years of diagnosis (Figure 1B).
CONCLUSION: We developed a new single ready-to-use risk model accounting for both IgM MGUS and SWM. Most IgM MGUS pts were categorized in the low-risk group, while SWM accounted for the vast majority of intermediate and high-risk groups. There were no differences in OS between IgM MGUS and SWM. However, RS of IgM MGUS was higher in the first 10 years from diagnosis, probably due to both early access to public health and follow-up, while SWM showed a constant decreasing RS.
Disclosures
Moreno:Janssen: Honoraria, Other: Travel grants. Bermúdez:Bristol Myers Squibb: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Speakers Bureau; GSK: Consultancy, Honoraria, Speakers Bureau; Neovii: Consultancy, Speakers Bureau; Trecondi: Consultancy, Speakers Bureau; MSD: Consultancy; Pfizer: Consultancy, Honoraria, Speakers Bureau. García-Sanz:Janssen: Honoraria, Other: Travel support, Research Funding; BeiGene: Honoraria, Other: Travel Support; Gilead: Honoraria, Research Funding; Astellas: Honoraria, Research Funding; Amgen: Honoraria; Takeda: Honoraria, Research Funding; GSK: Honoraria, Other: Travel Support; Astra Zeneca: Honoraria; In Vivo Scribe: Patents & Royalties: Indirect perception, Euroclonality primers; Novartis: Honoraria, Research Funding. Fernández De Larrea:Pfizer: Honoraria; Beigene: Consultancy, Honoraria; Sanofi: Consultancy; GSK: Honoraria; Takeda: Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; BMS: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal